Product Details
73-78-9 Properties
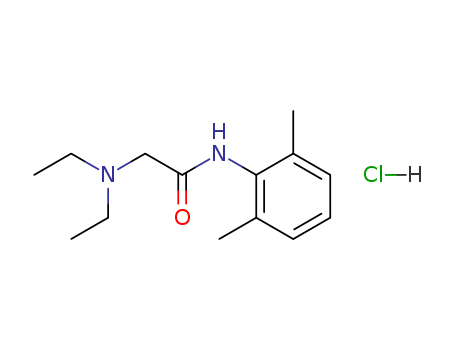
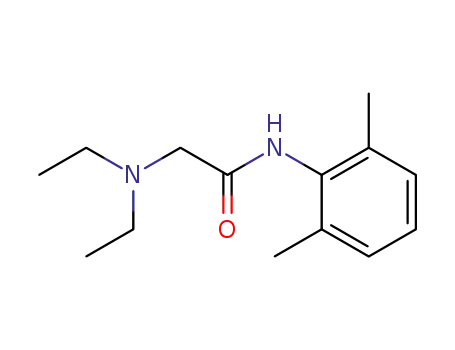
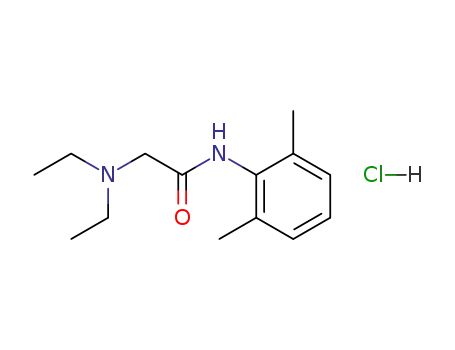
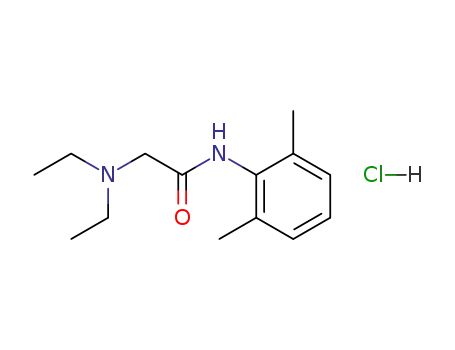
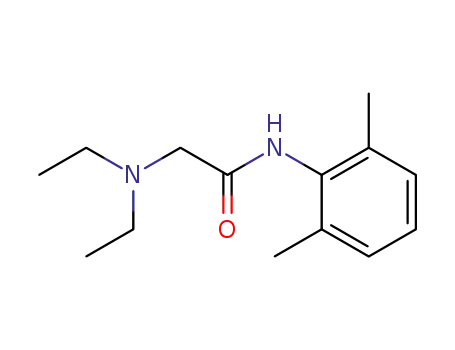
- Molecular Formula:C14H22N2O.HCl
- Molecular Weight:270.802
- Appearance/Colour:white crystal powder
- Vapor Pressure:4.28E-05mmHg at 25°C
- Melting Point:80-82 °C
- Boiling Point:350.8 °C at 760 mmHg
- Flash Point:166 °C
- PSA:32.34000
- LogP:3.45870
73-78-9 Usage
General
Lidocaine hydrochloride was synthesized by L?fgren and Lundquist in 1943, and was clinically introduced in 1948. It remains one of the most widely used local anaesthetics. It can be administered parenterally for a peripheral nerve block (PNB), intravenously, or applied topically at strengths of 2–4%. The addition of epinephrine 1:200 000 to 1:100 000 slows the vascular absorption of lidocaine and prolongs its effects.
Physical and chemical properties
Lidocaine hydrochloride is white and odorless crystal with bitter and numb taste. It is easily soluble in water, ethanol and organic solvents, but insoluble in ether. Aqueous solution in the case of acid and alkali do not break down, repeated autoclave rarely go bad.
Local anesthetic and antiarrhythmic drugs
Lidocaine hydrochloride is a local anesthetic and antiarrhythmic drug. It is clinically used for infiltration anesthesia, epidural anesthesia, surface anesthesia (including in the thoracoscopy or abdominal surgery for mucosal anesthesia) and nerve conduction block. The drug can also be used for acute myocardial infarction after ventricular premature beats and ventricular tachycardia, and for digitalis poisoning, cardiac surgery and ventricular arrhythmias caused by cardiac catheterization. But it is usually ineffective for supraventricular arrhythmias. Lidocaine hydrochloride is an amide local anesthetic. After blood absorption or intravenous administration, the drug has obvious excitement and inhibition of biphasic effects for the central nervous system, and no excitement of the pioneer. With the dose increased, the role or toxicity increased, there is an anti-convulsive effect with sub-poisoning plasma concentration; Blood concentration of more than 5μg ? ml-1 can occur convulsions. Lidocaine hydrochloride in low doses can promote outflow of K+ in cardiomyocytes, reduce myocardial autonomy, and has antiarrhythmic effects. In the treatment dose, lidocaine hydrochloride has no significant effect for the electrical activity of cardiomyocytes, atrioventricular conduction and myocardial contraction. Increased plasma concentration may cause slowing of heart conduction, atrioventricular block, inhibition of myocardial contractility and decreased cardiac output.
Application
Lidocaine hydrochloride is characterized by strong penetration, strong dispersion, rapidly onset. The anesthetic performance is twice that of procaine and the toxicity is1. There is an anesthetic effect after 5 minutes treatments, and anesthesia can last 1 to 1.5 hours, 50% longer than procaine. The drug is effective on the heart of the disease or arrhythmia caused by cardiac glycoside, but on the supraventricular tachycardia is poor. This product is fast and oral ineffective, with short duration, and often used as intravenous administration.
Metabolism
Lidocaine is metabolized by the liver with only a small amount (3%) found unchanged in urine. The three main mechanisms of metabolism are shown below: N-de-ethylation > monoethylglycinexylidide (MEGX) > glycinexylidide Hydrolysis of glycinexylidide 5-hydroxylation of lidocaine’s benzene ring Lidocaine possesses convulsant activity. Hepatic disease or reduced hepatic blood flow (as in congestive cardiac failure) will lower metabolic capacity.
Indications
The drug can be used for infiltration anesthesia, epidural anesthesia, surface anesthesia and nerve conduction block The drug can be used for acute myocardial infarction after ventricular premature beats and ventricular tachycardia, and for digitalis poisoning, cardiac surgery and ventricular arrhythmias caused by cardiac catheterization. But it is usually ineffective for supraventricular arrhythmias.
Usage and dosage
Surface anesthesia with solution of 2% to 5%.Infiltration anesthesia with solution of 0.25% to 0.5%, conduction anesthesia with 2%, each injection point, horse, cattle 8 to 12 ml, sheep 3 to 4 ml. Epidural anesthesia with 2% solution, horse, cow, 8 to 12 ml, dog, cat, 0.22 ml per kilogram of body weight. Subcutaneous injection with 2% solution, pig, sheep, 80 ml, horse, cow, 400 ml, dog,25 ml, cat, 8.5 ml. Treatment of arrhythmia, intravenous injection: Per kg of dog’s body weight of the initial dose is 2 to 4 mg, followed by 25 to 75 micrograms per minute intravenous infusion; Cat initial dose of 250 to 500 micrograms, followed by intravenous infusion of 20 micrograms per minute.
Adverse effect
The incidence of adverse effect with lidocaine hydrochloride was about 6.3%. Most adverse effects are dose dependent. Adverse effects are drowsiness, dizziness, nausea, vomiting, burnout, euphoria, insanity, muscle convulsions, syncope, blurred vision, confusion and difficulty breathing. Large doses lead to severe sinus bradycardia, cardiac arrest, severe atrioventricular block and weakened myocardial contractility, reduced blood pressure and so on. Excess concentrations of lidocaine hydrochloride in the blood cause some problems. For example, atrial conduction slows, atrioventricular blocks (A-V-B), and inhibits myocardial contractility and cardiac output decreases. There are little allergic effects, such as erythema rash, angioneurotic edema and so on.
Additional information
Lidocaine is contraindicated in patients with known hypersensitivity to local anaesthetics of the amide type and in patients with porphyria. Reactions due to overdose with lidocaine (high plasma levels) are systemic and involve the central nervous and cardiovascular systems. Effects include medullary depression, tonic and clonic convulsions, and cardiovascular collapse Solutions in multidose vials may contain hydrobenzoate derivatives and have been associated with allergic reactions in some patients. As with all of the amide local anaesthetics protein binding is reduced in the neonate (50% versus 64% in the adult), which necessitates reduced doses if adverse reactions are to be avoided.
Medicine interactions
Cimetidine and β-blockers can inhibit metabolism of lidocaine through liver, so that the blood concentration increases and adverse reactions occur in the heart and nervous system. We should adjust the dose of lidocaine hydrochloride. Barbiturates can promote the metabolism of lidocaine hydrochloride, and the two drugs can cause bradycardia and sinus arrest. Combined with procainamide, the drug can produce excessive delirium and hallucinations, but does not affect the product plasma concentration. Isoprenaline Isoprinosine could increase the total clearance of lidocaine hydrochloride through increased liver blood flow; norepinephrine could reduce the total clearance of lidocaine hydrochlor through reduced liver blood flow. The drug is contraindicated with phenobarbital, thiopental sodium, sodium nitroprusside, mannitol, amphotericin B, ampicillin, and sulfadiazine.
Precautions
Patients Allergic to other local anesthetics may be allergic to lidocaine hydrochloride. The following circumstances with caution: Pregnancy, neonatal especially in premature infants, liver blood flow reduction, liver and kidney dysfunction, congestive heart failure, severe myocardial damage, low blood volume, shock and other patients. Strictly grasp the concentration and total medication, excessive can cause convulsions and cardiac arrest; the body metabolism is slower than procaine, and there is accumulation, causing poisoning and convulsions. Medication of the elderly should be adjusted the dose according to the needs and tolerability, and over the age of 70 should be halved. Prevent straying into the blood vessels when anaesthetizing, prevent local anesthetic poisoning. ?We should pay attention to monitoring blood pressure, electrocardiogram, and with rescue equipment when arrhythmia Treatment; drug administration should be immediately discontinued in some circumstances. For example, ECG P-R interval prolongs or QRS wave widens, other arrhythmia or the original arrhythmia deteriorates.
References
https://www.drugbank.ca/drugs/DB00281 https://en.wikipedia.org/wiki/Lidocaine
Chemical Properties
White to Off-White Solid
Originator
Xylocaine,Astra,US,1949
Uses
Apply to affected site 5 to 10 minutes before procedure. Duration of anesthesia is relatively short (<1 hour).
Uses
Local anesthesic;Na+ channel blocker
Uses
Anesthetic (local); antiarrhythmic (class IB). Long-acting, membrane stabilizing agent against ventricular arrhythmia. Originally developed as a local anesthetic.
Definition
ChEBI: The anhydrous form of the hydrochloride salt of lidocaine.
Manufacturing Process
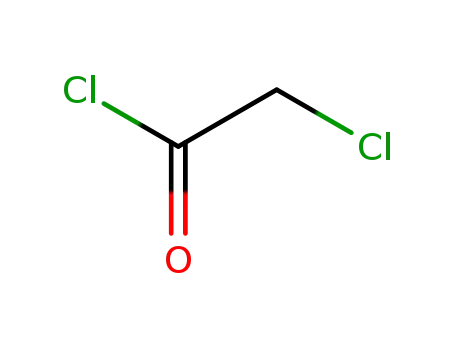
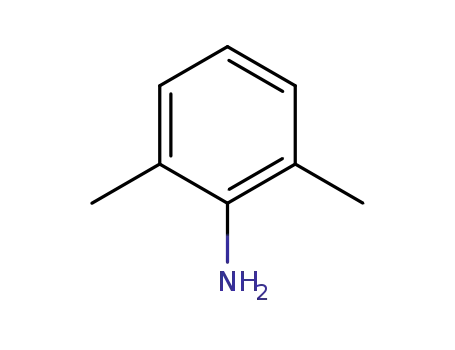
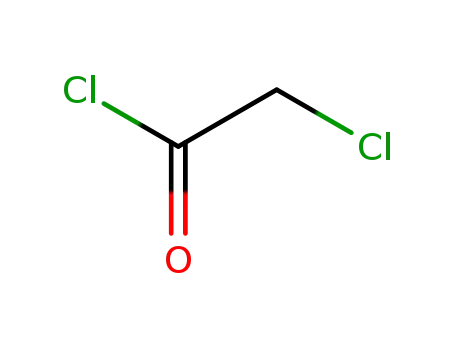
One mol of 2,6-xylidine is dissolved in 800 ml glacial acetic acid. The mixture is cooled to 10°C, after which 1.1 mol chloracetyl chloride is added at one time. The mixture is stirred vigorously during a few moments after which 1,000 ml half-saturated sodium acetate solution, or other buffering or alkalizing substance, is added at one time. The reaction mixture is shaken during half an hour. The precipitate formed which consists of ω-chloro-2,6- dimethyl-acetanilide is filtered off, washed with water and dried. The product is sufficiently pure for further treatment. The yield amounts to 70 to 80% of the theoretical amount.One mole of the chloracetyl xylidide thus prepared and 2.5 to 3 mols diethyl amine are dissolved in 1,000 ml dry benzene. The mixture is refluxed for 4 to 5 hours. The separated diethyl amine hydrochloride is filtered off. The benzene solution is shaken out two times with 3N hydrochloric acid, the first time with 800 ml and the second time with 400 ml acid. To the combined acid extracts is added an approximately 30% solution of sodium hydroxide until the precipitate does not increase.The precipitate, which sometimes is an oil, is taken up in ether. The ether solution is dried with anhydrous potassium carbonate after which the ether is driven off. The remaining crude substance is purified by vacuum distillation. During the distillation practically the entire quantity of the substance is carried over within a temperature interval of 1° to 2°C. The yield approaches the theoretical amount. MP 68° to 69°C. BP 180° to 182°C at 4 mm Hg; 159° to 160°C at 2 mm Hg. (Procedure is from US Patent 2,441,498.)
Brand name
Alpha caine Hydrochloride (Carlisle); Anestacon (Polymedica); Laryng-O-Jet (International Medication); Lidocaton (Phar maton); Lidopen (Meridian); Xylocaine (Abraxis); Xylo caine (AstraZeneca); Xylocaine (Dentsply).
Therapeutic Function
Local anesthetic, Antiarrhythmic
Biological Functions
Lidocaine hydrochloride (Xylocaine) is the most commonly used local anesthetic. It is well tolerated, and in addition to its use in infiltration and regional nerve blocks, it is commonly used for spinal and topical anesthesia and as an antiarrhythmic agent. Lidocaine has a more rapidly occurring, more intense, and more prolonged duration of action than does procaine.
General Description
Lidocaine hydrochloride,2-(diethylamino)-2 ,6 -acetoxylidide monohydrochloride(Xylocaine), was conceived as a derivative of gramine(3-dimethylaminomethylindole) and introduced as a localanesthetic. It is now being used intravenously as a standardparenteral agent for suppression of arrhythmias associatedwith acute myocardial infarction and cardiac surgery.It isthe drug of choice for the parenteral treatment of prematureventricular contractions.
Mechanism of action
Lidocaine can block Na+ and K+ ?ion channels and regulate intracellular and extracellular calcium ?concentrations through other ligand-gated ion channels. Lidocaine was ?the first sodium channel blocker to be identified. Its main mechanism of ?action is blocking voltage-gated Na+ channels (VGSC/NaVs).
Clinical Use
Lidocaine hydrochloride is a class IB antiarrhythmicagent with a different effect on the electrophysiologicalproperties of myocardial cells from that of procainamideand quinidine. It binds with equal affinity to the active (A)and inactive (I) Na+ ion channels. It depresses diastolic depolarizationand automaticity in the Purkinje fiber networkand increases the functional refractory period relative toaction potential duration, as do procainamide and quinidine.It differs from the latter two drugs, however, in that it doesnot decrease, and may even enhance, conduction velocity and increase membrane responsiveness to stimulation.There are fewer data available on the subcellular mechanismsresponsible for the antiarrhythmic actions of lidocainethan on the more established drug quinidine. It has been proposedthat lidocaine has little effect on membrane cation exchangeof the atria. Sodium ion entrance into ventricularcells during excitation is not influenced by lidocaine becauseit does not alter conduction velocity in this area.Lidocaine hydrochloride does depress Na+ influx duringdiastole, as do all other antiarrhythmic drugs, to diminishautomaticity in myocardial tissue. It also alters membraneresponsiveness in Purkinje fibers, allowing increased conductionvelocity and ample membrane potential at the timeof excitation.
Safety Profile
Poison by ingestion, intraperitoneal, intravenous, subcutaneous, intramuscular, and intratracheal routes. Human systemic effects: somnolence, respiratory depression, low blood pressure, cardiomyopathy includmg infarction, pulse rate increase. An experimental teratogen. Other experimental reproductive effects. A skin and eye irritant. An anesthetic. When heated to decomposition it emits very toxic fumes of NOx and HCl.
storage
Store in a tightly closed container at room temperature away from light and moisture. Do not store in the bathroom. Do not freeze. Keep all medications away from children and pets.
General
Lidocaine hydrochloride was synthesized by L?fgren and Lundquist in 1943, and was clinically introduced in 1948. It remains one of the most widely used local anaesthetics. It can be administered parenterally for a peripheral nerve block (PNB), intravenously, or applied topically at strengths of 2–4%. The addition of epinephrine 1:200 000 to 1:100 000 slows the vascular absorption of lidocaine and prolongs its effects.
Physical and chemical properties
Lidocaine hydrochloride is white and odorless crystal with bitter and numb taste. It is easily soluble in water, ethanol and organic solvents, but insoluble in ether. Aqueous solution in the case of acid and alkali do not break down, repeated autoclave rarely go bad.
Local anesthetic and antiarrhythmic drugs
Lidocaine hydrochloride is a local anesthetic and antiarrhythmic drug. It is clinically used for infiltration anesthesia, epidural anesthesia, surface anesthesia (including in the thoracoscopy or abdominal surgery for mucosal anesthesia) and nerve conduction block. The drug can also be used for acute myocardial infarction after ventricular premature beats and ventricular tachycardia, and for digitalis poisoning, cardiac surgery and ventricular arrhythmias caused by cardiac catheterization. But it is usually ineffective for supraventricular arrhythmias. Lidocaine hydrochloride is an amide local anesthetic. After blood absorption or intravenous administration, the drug has obvious excitement and inhibition of biphasic effects for the central nervous system, and no excitement of the pioneer. With the dose increased, the role or toxicity increased, there is an anti-convulsive effect with sub-poisoning plasma concentration; Blood concentration of more than 5μg ? ml-1 can occur convulsions. Lidocaine hydrochloride in low doses can promote outflow of K+ in cardiomyocytes, reduce myocardial autonomy, and has antiarrhythmic effects. In the treatment dose, lidocaine hydrochloride has no significant effect for the electrical activity of cardiomyocytes, atrioventricular conduction and myocardial contraction. Increased plasma concentration may cause slowing of heart conduction, atrioventricular block, inhibition of myocardial contractility and decreased cardiac output.
Application
Lidocaine hydrochloride is characterized by strong penetration, strong dispersion, rapidly onset. The anesthetic performance is twice that of procaine and the toxicity is1. There is an anesthetic effect after 5 minutes treatments, and anesthesia can last 1 to 1.5 hours, 50% longer than procaine. The drug is effective on the heart of the disease or arrhythmia caused by cardiac glycoside, but on the supraventricular tachycardia is poor. This product is fast and oral ineffective, with short duration, and often used as intravenous administration.
Metabolism
Lidocaine is metabolized by the liver with only a small amount (3%) found unchanged in urine. The three main mechanisms of metabolism are shown below: N-de-ethylation > monoethylglycinexylidide (MEGX) > glycinexylidide Hydrolysis of glycinexylidide 5-hydroxylation of lidocaine’s benzene ring Lidocaine possesses convulsant activity. Hepatic disease or reduced hepatic blood flow (as in congestive cardiac failure) will lower metabolic capacity.
Indications
The drug can be used for infiltration anesthesia, epidural anesthesia, surface anesthesia and nerve conduction block The drug can be used for acute myocardial infarction after ventricular premature beats and ventricular tachycardia, and for digitalis poisoning, cardiac surgery and ventricular arrhythmias caused by cardiac catheterization. But it is usually ineffective for supraventricular arrhythmias.
Usage and dosage
Surface anesthesia with solution of 2% to 5%.Infiltration anesthesia with solution of 0.25% to 0.5%, conduction anesthesia with 2%, each injection point, horse, cattle 8 to 12 ml, sheep 3 to 4 ml. Epidural anesthesia with 2% solution, horse, cow, 8 to 12 ml, dog, cat, 0.22 ml per kilogram of body weight. Subcutaneous injection with 2% solution, pig, sheep, 80 ml, horse, cow, 400 ml, dog,25 ml, cat, 8.5 ml. Treatment of arrhythmia, intravenous injection: Per kg of dog’s body weight of the initial dose is 2 to 4 mg, followed by 25 to 75 micrograms per minute intravenous infusion; Cat initial dose of 250 to 500 micrograms, followed by intravenous infusion of 20 micrograms per minute.
Adverse effect
The incidence of adverse effect with lidocaine hydrochloride was about 6.3%. Most adverse effects are dose dependent. Adverse effects are drowsiness, dizziness, nausea, vomiting, burnout, euphoria, insanity, muscle convulsions, syncope, blurred vision, confusion and difficulty breathing. Large doses lead to severe sinus bradycardia, cardiac arrest, severe atrioventricular block and weakened myocardial contractility, reduced blood pressure and so on. Excess concentrations of lidocaine hydrochloride in the blood cause some problems. For example, atrial conduction slows, atrioventricular blocks (A-V-B), and inhibits myocardial contractility and cardiac output decreases. There are little allergic effects, such as erythema rash, angioneurotic edema and so on.
Additional information
Lidocaine is contraindicated in patients with known hypersensitivity to local anaesthetics of the amide type and in patients with porphyria. Reactions due to overdose with lidocaine (high plasma levels) are systemic and involve the central nervous and cardiovascular systems. Effects include medullary depression, tonic and clonic convulsions, and cardiovascular collapse Solutions in multidose vials may contain hydrobenzoate derivatives and have been associated with allergic reactions in some patients. As with all of the amide local anaesthetics protein binding is reduced in the neonate (50% versus 64% in the adult), which necessitates reduced doses if adverse reactions are to be avoided.
Medicine interactions
Cimetidine and β-blockers can inhibit metabolism of lidocaine through liver, so that the blood concentration increases and adverse reactions occur in the heart and nervous system. We should adjust the dose of lidocaine hydrochloride. Barbiturates can promote the metabolism of lidocaine hydrochloride, and the two drugs can cause bradycardia and sinus arrest. Combined with procainamide, the drug can produce excessive delirium and hallucinations, but does not affect the product plasma concentration. Isoprenaline Isoprinosine could increase the total clearance of lidocaine hydrochloride through increased liver blood flow; norepinephrine could reduce the total clearance of lidocaine hydrochlor through reduced liver blood flow. The drug is contraindicated with phenobarbital, thiopental sodium, sodium nitroprusside, mannitol, amphotericin B, ampicillin, and sulfadiazine.
Precautions
Patients Allergic to other local anesthetics may be allergic to lidocaine hydrochloride. The following circumstances with caution: Pregnancy, neonatal especially in premature infants, liver blood flow reduction, liver and kidney dysfunction, congestive heart failure, severe myocardial damage, low blood volume, shock and other patients. Strictly grasp the concentration and total medication, excessive can cause convulsions and cardiac arrest; the body metabolism is slower than procaine, and there is accumulation, causing poisoning and convulsions. Medication of the elderly should be adjusted the dose according to the needs and tolerability, and over the age of 70 should be halved. Prevent straying into the blood vessels when anaesthetizing, prevent local anesthetic poisoning. ?We should pay attention to monitoring blood pressure, electrocardiogram, and with rescue equipment when arrhythmia Treatment; drug administration should be immediately discontinued in some circumstances. For example, ECG P-R interval prolongs or QRS wave widens, other arrhythmia or the original arrhythmia deteriorates.
References
https://www.drugbank.ca/drugs/DB00281 https://en.wikipedia.org/wiki/Lidocaine
Chemical Properties
White to Off-White Solid
Originator
Xylocaine,Astra,US,1949
Uses
Apply to affected site 5 to 10 minutes before procedure. Duration of anesthesia is relatively short (<1 hour).
Uses
Local anesthesic;Na+ channel blocker
Uses
Anesthetic (local); antiarrhythmic (class IB). Long-acting, membrane stabilizing agent against ventricular arrhythmia. Originally developed as a local anesthetic.
Definition
ChEBI: The anhydrous form of the hydrochloride salt of lidocaine.
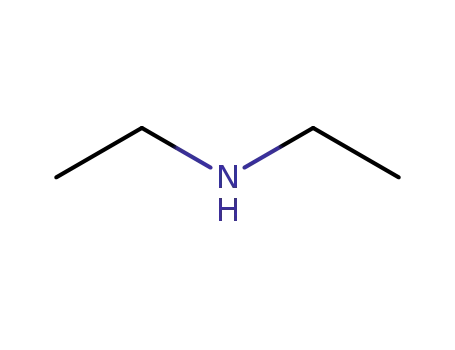
Manufacturing Process
One mol of 2,6-xylidine is dissolved in 800 ml glacial acetic acid. The mixture is cooled to 10°C, after which 1.1 mol chloracetyl chloride is added at one time. The mixture is stirred vigorously during a few moments after which 1,000 ml half-saturated sodium acetate solution, or other buffering or alkalizing substance, is added at one time. The reaction mixture is shaken during half an hour. The precipitate formed which consists of ω-chloro-2,6- dimethyl-acetanilide is filtered off, washed with water and dried. The product is sufficiently pure for further treatment. The yield amounts to 70 to 80% of the theoretical amount.One mole of the chloracetyl xylidide thus prepared and 2.5 to 3 mols diethyl amine are dissolved in 1,000 ml dry benzene. The mixture is refluxed for 4 to 5 hours. The separated diethyl amine hydrochloride is filtered off. The benzene solution is shaken out two times with 3N hydrochloric acid, the first time with 800 ml and the second time with 400 ml acid. To the combined acid extracts is added an approximately 30% solution of sodium hydroxide until the precipitate does not increase.The precipitate, which sometimes is an oil, is taken up in ether. The ether solution is dried with anhydrous potassium carbonate after which the ether is driven off. The remaining crude substance is purified by vacuum distillation. During the distillation practically the entire quantity of the substance is carried over within a temperature interval of 1° to 2°C. The yield approaches the theoretical amount. MP 68° to 69°C. BP 180° to 182°C at 4 mm Hg; 159° to 160°C at 2 mm Hg. (Procedure is from US Patent 2,441,498.)
Brand name
Alpha caine Hydrochloride (Carlisle); Anestacon (Polymedica); Laryng-O-Jet (International Medication); Lidocaton (Phar maton); Lidopen (Meridian); Xylocaine (Abraxis); Xylo caine (AstraZeneca); Xylocaine (Dentsply).
Therapeutic Function
Local anesthetic, Antiarrhythmic
Biological Functions
Lidocaine hydrochloride (Xylocaine) is the most commonly used local anesthetic. It is well tolerated, and in addition to its use in infiltration and regional nerve blocks, it is commonly used for spinal and topical anesthesia and as an antiarrhythmic agent. Lidocaine has a more rapidly occurring, more intense, and more prolonged duration of action than does procaine.
General Description
Lidocaine hydrochloride,2-(diethylamino)-2 ,6 -acetoxylidide monohydrochloride(Xylocaine), was conceived as a derivative of gramine(3-dimethylaminomethylindole) and introduced as a localanesthetic. It is now being used intravenously as a standardparenteral agent for suppression of arrhythmias associatedwith acute myocardial infarction and cardiac surgery.It isthe drug of choice for the parenteral treatment of prematureventricular contractions.
Mechanism of action
Lidocaine can block Na+ and K+ ?ion channels and regulate intracellular and extracellular calcium ?concentrations through other ligand-gated ion channels. Lidocaine was ?the first sodium channel blocker to be identified. Its main mechanism of ?action is blocking voltage-gated Na+ channels (VGSC/NaVs).
Clinical Use
Lidocaine hydrochloride is a class IB antiarrhythmicagent with a different effect on the electrophysiologicalproperties of myocardial cells from that of procainamideand quinidine. It binds with equal affinity to the active (A)and inactive (I) Na+ ion channels. It depresses diastolic depolarizationand automaticity in the Purkinje fiber networkand increases the functional refractory period relative toaction potential duration, as do procainamide and quinidine.It differs from the latter two drugs, however, in that it doesnot decrease, and may even enhance, conduction velocity and increase membrane responsiveness to stimulation.There are fewer data available on the subcellular mechanismsresponsible for the antiarrhythmic actions of lidocainethan on the more established drug quinidine. It has been proposedthat lidocaine has little effect on membrane cation exchangeof the atria. Sodium ion entrance into ventricularcells during excitation is not influenced by lidocaine becauseit does not alter conduction velocity in this area.Lidocaine hydrochloride does depress Na+ influx duringdiastole, as do all other antiarrhythmic drugs, to diminishautomaticity in myocardial tissue. It also alters membraneresponsiveness in Purkinje fibers, allowing increased conductionvelocity and ample membrane potential at the timeof excitation.
Safety Profile
Poison by ingestion, intraperitoneal, intravenous, subcutaneous, intramuscular, and intratracheal routes. Human systemic effects: somnolence, respiratory depression, low blood pressure, cardiomyopathy includmg infarction, pulse rate increase. An experimental teratogen. Other experimental reproductive effects. A skin and eye irritant. An anesthetic. When heated to decomposition it emits very toxic fumes of NOx and HCl.
storage
Store in a tightly closed container at room temperature away from light and moisture. Do not store in the bathroom. Do not freeze. Keep all medications away from children and pets.
InChI:InChI=1/C14H22N2O.ClH/c1-5-16(6-2)10-13(17)15-14-11(3)8-7-9-12(14)4;/h7-9H,5-6,10H2,1-4H3,(H,15,17);1H
73-78-9 Relevant articles
The molecular structure and vibrational, 1H and 13C NMR spectra of lidocaine hydrochloride monohydrate
Badawi, Hassan M.,F?rner, Wolfgang,Ali, Shaikh A.
, p. 92 - 100 (2016)
The structure, vibrational and NMR spectra of the local anesthetic drug lidocaine hydrochloride monohydrate salt were investigated by B3LYP/6-311G calculations. The lidocaine·HCl·H2O salt is predicted to have the gauche structure as the predominant form at ambient temperature with NCCN and CNCC torsional angles of 110° and -123° as compared to 10° and -64°, respectively in the base lidocaine. The repulsive interaction between the two N-H bonds destabilized the gauche structure of lidocaine·HCl·H2O salt. The analysis of the observed vibrational spectra is consistent with the presence of the lidocaine salt in only one gauche conformation at room temperature. The 1H and 13C NMR spectra of lidocaine·HCl·H2O were interpreted by experimental and DFT calculated chemical shifts of the lidocaine salt. The RMSD between experimental and theoretical 1H and 13C chemical shifts for lidocaine·HCl·H2O is 2.32 and 8.21 ppm, respectively.
Preparation method of lidocaine hydrochloride
-
Paragraph 0031; 0037-0038, (2020/01/25)
The invention relates to a preparation method of lidocaine hydrochloride, which comprises the following steps: carrying out acylation reaction by using 2, 6-dimethylaniline and chloroacetyl chloride as raw materials, directly adding diethylamine into the system to carry out amination reaction after the reaction is finished, filtering the product, and adding hydrochloric acid into the filtrate to carry out salification reaction. The preparation method of lidocaine hydrochloride provided by the invention is a one-pot method, avoids repeated purification of an intermediate product in a traditional process, and is simple in process, mild in condition, easy to control, high in product yield and high in purity.
Method for preparing lidocaine hydrochloride
-
Paragraph 0028; 0030, (2016/11/28)
The invention provides a method for preparing lidocaine hydrochloride, and belongs to the technical field of anesthetic synthesis. The method comprises the following steps: by taking 2,6-xylenol as a raw material, Pd/C as a main catalyst and 2,6-dimethylcyclohexanone as a promoter, performing liquid phase amination with ammonia water at high temperature, thereby obtaining a midbody 2,6-dimethylaniline; enabling sodium methylate, 2,6-dimethylaniline and N,N-lignocaine methyl acetate as raw materials to react at 90-95 DEGC, distilling while reaction is performed to remove methanol till no methanol can be evaporated out, continuously reacting for 30 minutes, cooling to the room temperature, adding dichloroethane, washing with water, and leaving to stand to layer, thereby obtaining an organic layer, namely, a lidocaine based dichloroethane solution; further adding hydrochloric acid into the lidocaine based dichloroethane solution, adjusting the pH value to be 3.5-4 by using hydrogen chloride, adding activated carbon to reflux for 20-40 minutes, filtering, concentrating the filtrate, cooling, crystallizing, and dying, thereby obtaining lidocaine hydrochloride. The lidocaine hydrochloride prepared by using the method is simple in synthesis process and high in product purity, that is, the purity can be greater than 99%, and the total yield is greater than 84%.
On-demand continuous-flow production of pharmaceuticals in a compact, reconfigurable system
Adamo, Andrea,Beingessner, Rachel L.,Behnam, Mohsen,Chen, Jie,Jamison, Timothy F.,Jensen, Klavs F.,Monbaliu, Jean-Christophe M.,Myerson, Allan S.,Revalor, Eve M.,Snead, David R.,Stelzer, Torsten,Weeranoppanant, Nopphon,Wong, Shin Yee,Zhang, Ping
, p. 61 - 67 (2016/04/26)
Pharmaceutical manufacturing typically uses batch processing at multiple locations. Disadvantages of this approach include long production times and the potential for supply chain disruptions. As a preliminary demonstration of an alternative approach, we report here the continuous-flow synthesis and formulation of active pharmaceutical ingredients in a compact, reconfigurable manufacturing platform. Continuous end-to-end synthesis in the refrigerator-sized [1.0 meter (width) × 0.7 meter (length) × 1.8 meter (height)] system produces sufficient quantities per day to supply hundreds to thousands of oral or topical liquid doses of diphenhydramine hydrochloride, lidocaine hydrochloride, diazepam, and fluoxetine hydrochloride that meet U.S. Pharmacopeia standards. Underlying this flexible plug-and-play approach are substantial enabling advances in continuous-flow synthesis, complex multistep sequence telescoping, reaction engineering equipment, and real-time formulation.
73-78-9 Process route
-
-
137-58-6
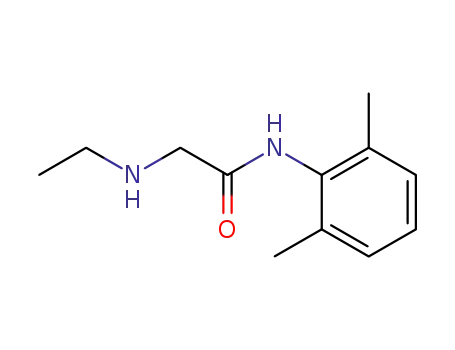
2-diethylamino-N-(2,6-dimethylphenyl)-acetamide

-
-
73-78-9
lidocaine hydrochloride
| Conditions | Yield |
|---|---|
|
With
hydrogenchloride;
In
diethyl ether;
|
100% |
|
With
hydrogenchloride; pyrographite;
In
water; 1,2-dichloro-ethane;
for 0.333333h;
pH=3.5;
pH-value;
|
88.72% |
|
With
hydrogenchloride;
In
water; acetone;
at 20 ℃;
pH=<= 4;
|
80.6% |
-
-
109-89-7
diethylamine

-
-
79-04-9
chloroacetyl chloride

-
-
87-62-7
2,6-dimethylaniline

-
-
73-78-9
lidocaine hydrochloride
| Conditions | Yield |
|---|---|
|
chloroacetyl chloride; 2,6-dimethylaniline;
In
1-methyl-pyrrolidin-2-one; methanol; water;
at 120 ℃;
for 0.306667h;
Flow reactor;
diethylamine;
With
potassium hydroxide;
In
methanol; water;
at 130 ℃;
for 0.295h;
under 12751.3 Torr;
Flow reactor;
With
hydrogenchloride;
In
methanol; diethyl ether; water;
|
73-78-9 Upstream products
-
137-58-6
2-diethylamino-N-(2,6-dimethylphenyl)-acetamide
-
109-89-7
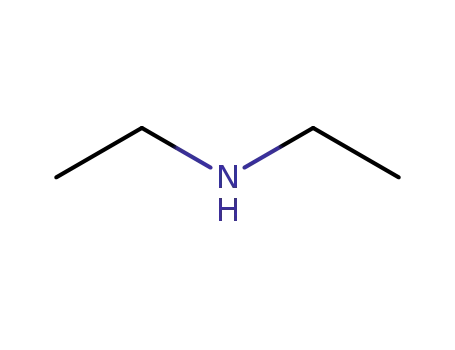
diethylamine
-
79-04-9
chloroacetyl chloride
-
87-62-7
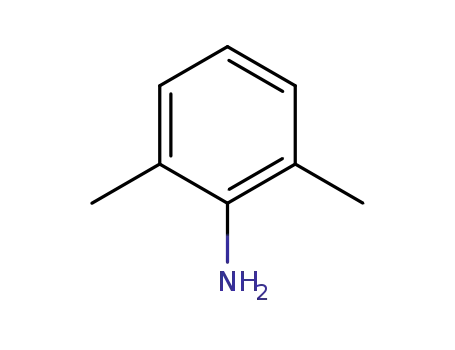
2,6-dimethylaniline
73-78-9 Downstream products
-
1220976-13-5
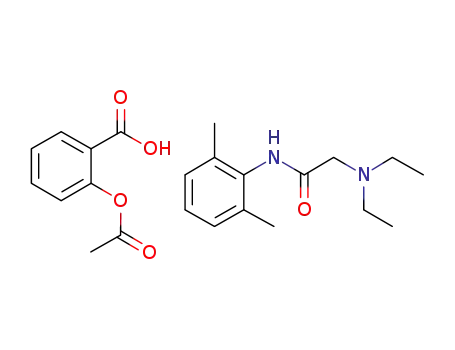
lidocainium acetylsalicylate
-
7728-40-7
N-(2,6-dimethylphenyl)-2-ethylaminoacetamide
-
32845-42-4
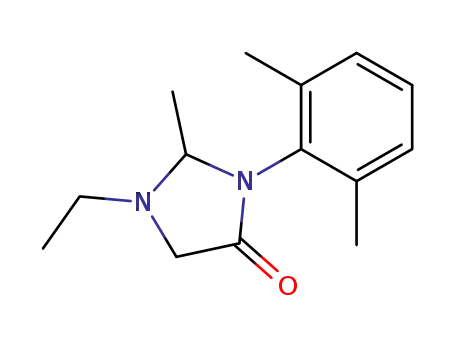
1-ethyl-2-methyl-3-(2,6-dimethylphenyl)imidazolidin-4-one
-
1158170-79-6
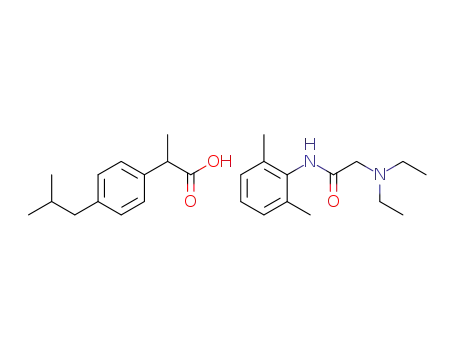
lidocainium ibuprofenate








